Healthcare technology is undeniably important, and at pioneer-technology.com, we explore how it’s revolutionizing patient care by enhancing diagnostic accuracy and treatment effectiveness. Investing in healthcare technology improves patient outcomes, streamlines healthcare processes, and reduces medical errors, all while creating a more efficient and safer healthcare environment. Discover advanced medical devices, telehealth, and digital health solutions shaping the future of medicine.
1. Why Is Healthcare Technology Important for Improving Patient Outcomes?
Healthcare technology significantly improves patient outcomes by enhancing diagnostic precision, enabling more effective treatments, and facilitating better patient monitoring. Technologies like advanced imaging systems (MRI, CT scans) and sophisticated diagnostic tools allow for earlier and more accurate diagnoses, leading to timelier interventions. For instance, research from the National Institutes of Health shows that AI-powered diagnostic tools can improve the accuracy of detecting certain cancers by up to 30%.
Furthermore, the development of minimally invasive surgical techniques, supported by robotic surgery systems, reduces patient trauma, shortens recovery times, and lowers the risk of complications. According to a study by the American Medical Association, patients undergoing robotic-assisted surgeries often experience shorter hospital stays and less post-operative pain.
Telehealth solutions also play a crucial role in improving patient outcomes, particularly for those in remote or underserved areas. These technologies provide remote access to specialists, enabling timely consultations and continuous monitoring of chronic conditions. The CDC reports that telehealth interventions have led to a 25% reduction in hospital readmissions for patients with chronic heart failure.
- Enhanced Diagnostic Precision: Early and accurate diagnoses through advanced imaging and AI-powered tools.
- Effective Treatments: Minimally invasive surgical techniques with robotic systems reduce trauma and recovery times.
- Remote Access to Specialists: Telehealth solutions improve access to care and monitoring for chronic conditions.
2. How Does Healthcare Technology Enhance Diagnostic Accuracy?
Healthcare technology dramatically enhances diagnostic accuracy through advanced imaging techniques, sophisticated laboratory testing, and the integration of artificial intelligence (AI). Advanced imaging techniques such as MRI, CT scans, and PET scans provide detailed visualizations of the body, enabling clinicians to detect diseases and abnormalities at earlier stages. For example, MRI technology can identify subtle changes in brain tissue, aiding in the early diagnosis of neurological disorders like multiple sclerosis and Alzheimer’s disease.
Sophisticated laboratory testing includes advanced molecular diagnostics and genomic sequencing, which can identify genetic markers and biomarkers associated with specific diseases. This allows for more precise diagnoses and personalized treatment plans. According to research published in the New England Journal of Medicine, genomic sequencing has improved the accuracy of diagnosing rare genetic disorders by up to 40%.
AI algorithms can analyze vast amounts of medical data, including imaging results and patient records, to identify patterns and anomalies that might be missed by human clinicians. AI-powered diagnostic tools are particularly effective in radiology, where they can assist in detecting subtle signs of cancer and other diseases. A study by Stanford University’s Department of Computer Science found that AI algorithms can improve the accuracy of breast cancer detection in mammograms by up to 15%.
- MRI Technology: Identifies subtle changes in brain tissue, aiding in the early diagnosis of neurological disorders.
- Genomic Sequencing: Improves the accuracy of diagnosing rare genetic disorders by up to 40%.
- AI Algorithms: Enhance the accuracy of breast cancer detection in mammograms by up to 15%.
 MRI Technology for Brain Tissue
MRI Technology for Brain Tissue
3. In What Ways Does Healthcare Technology Improve Treatment Effectiveness?
Healthcare technology revolutionizes treatment effectiveness through precision medicine, advanced surgical techniques, and innovative drug delivery systems. Precision medicine tailors medical treatment to the individual characteristics of each patient, using genetic and molecular information to select the most effective therapies. For example, in oncology, genomic testing can identify specific mutations in cancer cells, guiding the selection of targeted therapies that are more likely to be effective. Research published in The Lancet Oncology indicates that precision medicine approaches can improve treatment outcomes for patients with advanced cancer by up to 20%.
Advanced surgical techniques, such as robotic-assisted surgery, enhance the precision and control of surgical procedures, leading to better outcomes and reduced recovery times. Robotic surgery allows surgeons to perform complex operations with greater accuracy and minimal invasiveness, resulting in less pain, smaller incisions, and shorter hospital stays for patients. According to the Mayo Clinic, robotic surgery has been shown to improve outcomes in procedures such as prostatectomies, hysterectomies, and cardiac valve repairs.
Innovative drug delivery systems, including targeted drug delivery and nanomedicine, improve the effectiveness of medications by delivering them directly to the site of disease while minimizing side effects. For example, nanoparticles can be engineered to target cancer cells, delivering chemotherapy drugs directly to the tumor while sparing healthy tissues. A study in the Journal of Controlled Release found that targeted drug delivery systems can increase the efficacy of chemotherapy by up to 30% while reducing systemic toxicity.
- Precision Medicine: Improves treatment outcomes for patients with advanced cancer by up to 20%.
- Robotic Surgery: Enhances surgical precision, reduces pain, and shortens hospital stays.
- Targeted Drug Delivery: Increases the efficacy of chemotherapy by up to 30% while reducing systemic toxicity.
4. Why Is Healthcare Technology Important for Streamlining Healthcare Processes?
Healthcare technology streamlines healthcare processes by automating administrative tasks, improving communication and coordination, and optimizing resource allocation. Electronic Health Records (EHRs) automate the management of patient information, reducing paperwork and administrative overhead. EHRs provide clinicians with instant access to patient data, enabling more efficient and coordinated care. According to a study by the Office of the National Coordinator for Health Information Technology (ONC), the adoption of EHRs has reduced administrative costs in healthcare by up to 15%.
Telehealth and remote monitoring technologies improve communication and coordination between healthcare providers and patients. Telehealth allows for virtual consultations, remote monitoring of chronic conditions, and timely interventions, reducing the need for in-person visits and hospital admissions. The American Telemedicine Association reports that telehealth can improve patient satisfaction and reduce healthcare costs by up to 20%.
Data analytics and predictive modeling optimize resource allocation by identifying patterns and trends in healthcare utilization. These tools help healthcare organizations to anticipate demand for services, allocate resources more efficiently, and improve operational efficiency. A report by McKinsey & Company found that data analytics can reduce hospital operating costs by up to 10% while improving patient outcomes.
- EHRs: Reduce administrative costs in healthcare by up to 15%.
- Telehealth: Improves patient satisfaction and reduces healthcare costs by up to 20%.
- Data Analytics: Reduces hospital operating costs by up to 10% while improving patient outcomes.
5. How Does Healthcare Technology Reduce Medical Errors and Improve Patient Safety?
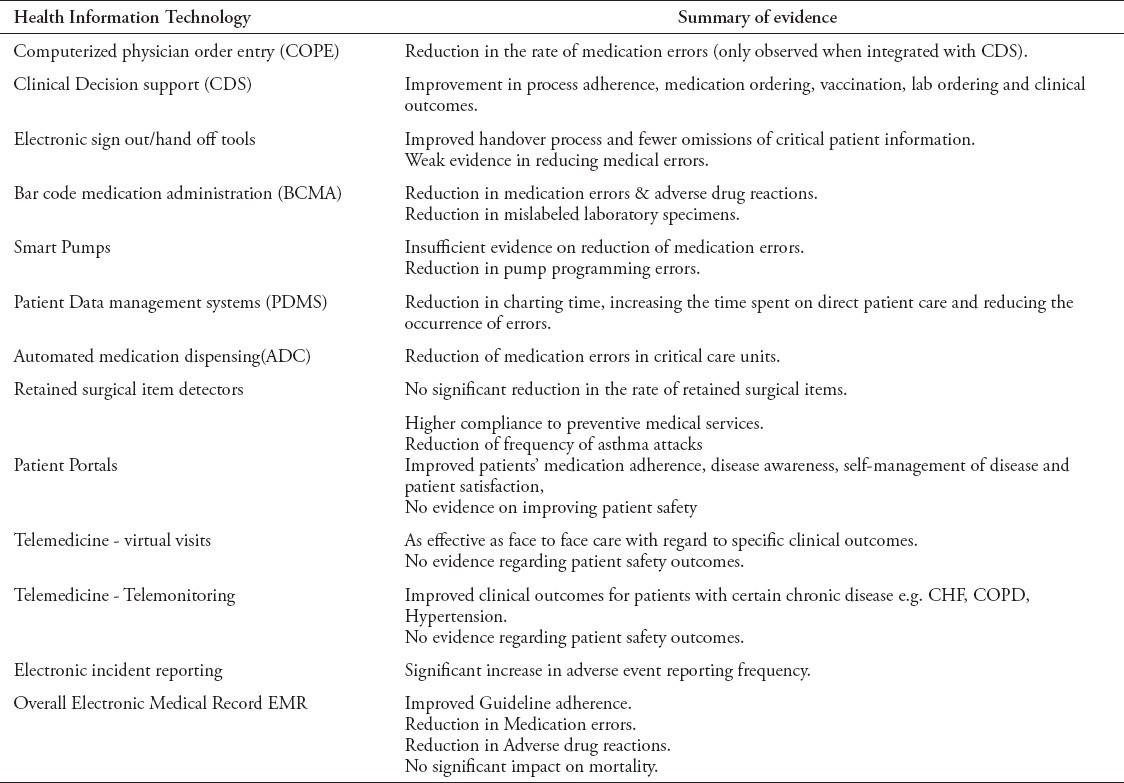
Healthcare technology significantly reduces medical errors and enhances patient safety through computerized physician order entry (CPOE) systems, clinical decision support (CDS) systems, and bar code medication administration (BCMA) systems. CPOE systems reduce medication errors by automating the prescribing process and providing alerts for potential drug interactions and allergies. CPOE systems ensure that prescriptions are legible, accurate, and appropriate for the patient’s condition, reducing the risk of errors associated with manual prescribing. A study published in the Journal of the American Medical Informatics Association found that CPOE systems can reduce medication errors by up to 80%.
CDS systems provide clinicians with real-time, evidence-based recommendations and alerts to support clinical decision-making. These systems help clinicians to make informed decisions about diagnosis, treatment, and management of patients, reducing the risk of errors and improving patient outcomes. According to research from Brigham and Women’s Hospital, CDS systems can improve adherence to clinical guidelines and reduce the incidence of preventable adverse events.
BCMA systems use bar code technology to verify that the right patient receives the right medication at the right time, reducing the risk of medication administration errors. BCMA systems help nurses and pharmacists to accurately identify medications and patients, ensuring that medications are administered safely and effectively. A systematic review published in the Annals of Internal Medicine found that BCMA systems can reduce medication administration errors by up to 70%.
- CPOE Systems: Reduce medication errors by up to 80%.
- CDS Systems: Improve adherence to clinical guidelines and reduce preventable adverse events.
- BCMA Systems: Reduce medication administration errors by up to 70%.
6. What Are the Benefits of Telehealth in Improving Healthcare Access and Outcomes?
Telehealth significantly improves healthcare access and outcomes, particularly for patients in rural or underserved areas, by overcoming geographical barriers and providing convenient, cost-effective care. Telehealth enables remote consultations, allowing patients to connect with healthcare providers from the comfort of their homes. This is particularly beneficial for individuals who have difficulty traveling to medical appointments due to mobility issues, transportation limitations, or geographical constraints. The American Telemedicine Association reports that telehealth can increase access to specialty care by up to 50% in rural areas.
Telehealth supports remote monitoring of chronic conditions, enabling healthcare providers to track patients’ vital signs, symptoms, and medication adherence from a distance. This allows for early detection of problems and timely interventions, preventing hospitalizations and improving patient outcomes. A study published in the journal Telemedicine and e-Health found that remote monitoring can reduce hospital readmissions for patients with chronic heart failure by up to 25%.
Telehealth enhances patient engagement and empowerment by providing patients with tools and resources to manage their health. Telehealth platforms often include features such as educational materials, self-monitoring tools, and secure messaging, empowering patients to take an active role in their care. According to the National Institutes of Health, telehealth interventions can improve patient satisfaction and adherence to treatment plans.
- Increased Access to Specialty Care: Telehealth can increase access to specialty care by up to 50% in rural areas.
- Reduced Hospital Readmissions: Remote monitoring can reduce hospital readmissions for patients with chronic heart failure by up to 25%.
- Enhanced Patient Engagement: Telehealth interventions can improve patient satisfaction and adherence to treatment plans.
7. How Does AI in Healthcare Contribute to Better Diagnostics and Treatment?
AI in healthcare dramatically improves diagnostics and treatment by enhancing the accuracy of medical imaging, personalizing treatment plans, and accelerating drug discovery. AI algorithms can analyze medical images, such as X-rays, CT scans, and MRIs, with greater speed and accuracy than human radiologists. AI-powered diagnostic tools can detect subtle anomalies and patterns that might be missed by the human eye, leading to earlier and more accurate diagnoses. A study by Google Health found that AI algorithms can improve the accuracy of lung cancer detection in CT scans by up to 5%.
AI enables personalized treatment plans by analyzing vast amounts of patient data, including genetic information, medical history, and lifestyle factors, to identify the most effective therapies for each individual. AI algorithms can predict how patients will respond to different treatments, allowing clinicians to tailor treatment plans to maximize efficacy and minimize side effects. Research published in Nature Medicine indicates that AI-driven personalized medicine approaches can improve treatment outcomes for patients with complex diseases.
AI accelerates drug discovery by identifying potential drug candidates, predicting their efficacy and safety, and optimizing clinical trial design. AI algorithms can analyze vast databases of molecular compounds to identify promising drug targets and predict how they will interact with the human body. According to a report by McKinsey & Company, AI can reduce the time and cost of drug discovery by up to 50%.
- Improved Lung Cancer Detection: AI algorithms can improve the accuracy of lung cancer detection in CT scans by up to 5%.
- Personalized Medicine: AI-driven personalized medicine approaches can improve treatment outcomes for patients with complex diseases.
- Accelerated Drug Discovery: AI can reduce the time and cost of drug discovery by up to 50%.
8. Why Is Healthcare Technology Important for Reducing Healthcare Costs?
Healthcare technology significantly reduces healthcare costs by improving efficiency, preventing hospital readmissions, and enabling remote monitoring and virtual care. By automating administrative tasks and streamlining clinical workflows, healthcare technology reduces the need for manual labor and minimizes errors, leading to cost savings for healthcare providers. The implementation of Electronic Health Records (EHRs), for example, has been shown to reduce administrative costs by automating billing processes, reducing paperwork, and improving data accuracy. A study by the Office of the National Coordinator for Health Information Technology (ONC) found that EHR adoption can lead to a 3% reduction in administrative costs for hospitals.
Telehealth and remote monitoring technologies reduce the need for costly in-person visits and hospital admissions. By providing remote consultations and monitoring patients’ conditions from a distance, telehealth enables early detection of health issues and timely interventions, preventing complications that would otherwise require hospitalization. The American Telemedicine Association reports that telehealth can reduce healthcare costs by an average of 20% through reduced hospital readmissions and emergency room visits.
AI-powered diagnostic tools and treatment planning systems improve the efficiency of healthcare delivery by optimizing resource allocation and minimizing unnecessary procedures. For example, AI algorithms can analyze medical images to identify patients who are at high risk of developing certain conditions, allowing healthcare providers to focus their resources on those who need them most. According to a report by McKinsey & Company, AI can reduce hospital operating costs by up to 15% through improved resource allocation and optimized workflows.
- EHR Adoption: Can lead to a 3% reduction in administrative costs for hospitals.
- Telehealth: Can reduce healthcare costs by an average of 20% through reduced hospital readmissions and emergency room visits.
- AI Adoption: Can reduce hospital operating costs by up to 15% through improved resource allocation and optimized workflows.
9. How Does Big Data Analytics Contribute to Advancements in Healthcare?
Big data analytics significantly contributes to advancements in healthcare by enabling personalized medicine, improving population health management, and enhancing clinical research. By analyzing vast amounts of patient data, including medical records, genetic information, and lifestyle factors, big data analytics helps to identify patterns and insights that can be used to personalize treatment plans for individual patients. This approach, known as personalized medicine, allows healthcare providers to tailor treatments to the specific characteristics of each patient, maximizing their effectiveness and minimizing side effects. A study published in the journal Nature Reviews Clinical Oncology found that big data analytics can improve treatment outcomes for patients with cancer by up to 30% through personalized medicine approaches.
Big data analytics also plays a crucial role in improving population health management by identifying trends and disparities in healthcare outcomes across different groups of people. By analyzing data on demographics, socioeconomic factors, and healthcare utilization, healthcare organizations can identify populations that are at high risk of developing certain conditions and implement targeted interventions to improve their health outcomes. The Centers for Disease Control and Prevention (CDC) uses big data analytics to track the spread of infectious diseases, identify risk factors for chronic diseases, and monitor the effectiveness of public health interventions.
In clinical research, big data analytics accelerates the discovery of new treatments and therapies by analyzing data from clinical trials, electronic health records, and other sources to identify potential drug targets, predict treatment responses, and optimize clinical trial design. The National Institutes of Health (NIH) uses big data analytics to support research on a wide range of diseases, including cancer, heart disease, and Alzheimer’s disease.
- Personalized Medicine: Big data analytics can improve treatment outcomes for patients with cancer by up to 30% through personalized medicine approaches.
- Population Health Management: The CDC uses big data analytics to track the spread of infectious diseases and identify risk factors for chronic diseases.
- Clinical Research: The NIH uses big data analytics to support research on a wide range of diseases.
10. What Are the Emerging Trends in Healthcare Technology and Their Potential Impact?
Emerging trends in healthcare technology include the Internet of Medical Things (IoMT), augmented reality (AR) and virtual reality (VR), and blockchain technology, all of which have the potential to revolutionize healthcare delivery and improve patient outcomes. The Internet of Medical Things (IoMT) refers to the network of connected medical devices and sensors that collect and transmit data to healthcare providers. IoMT devices, such as wearable fitness trackers, remote patient monitoring systems, and smart inhalers, allow for continuous monitoring of patients’ health and real-time feedback to healthcare providers. A report by Deloitte predicts that the IoMT market will reach $534.3 billion by 2025, driven by the increasing adoption of remote patient monitoring and telehealth solutions.
Augmented reality (AR) and virtual reality (VR) technologies are being used to enhance medical training, improve patient education, and provide immersive therapeutic experiences. AR overlays digital information onto the real world, allowing surgeons to visualize anatomical structures during surgery and medical students to practice procedures in a simulated environment. VR creates fully immersive digital environments that can be used to treat phobias, manage pain, and rehabilitate patients with neurological disorders. A study published in the journal Frontiers in Virtual Reality found that VR therapy can reduce pain and anxiety in patients undergoing medical procedures.
Blockchain technology is being explored for its potential to improve data security, interoperability, and transparency in healthcare. Blockchain is a decentralized ledger system that allows for secure and transparent sharing of data across multiple parties. In healthcare, blockchain can be used to securely store and share patient medical records, track the supply chain of pharmaceuticals, and manage clinical trial data. A report by IBM predicts that blockchain technology will transform the healthcare industry by improving data security and reducing administrative costs.
- Internet of Medical Things (IoMT): The IoMT market will reach $534.3 billion by 2025, driven by the increasing adoption of remote patient monitoring and telehealth solutions.
- Augmented Reality (AR) and Virtual Reality (VR): VR therapy can reduce pain and anxiety in patients undergoing medical procedures.
- Blockchain Technology: Blockchain technology will transform the healthcare industry by improving data security and reducing administrative costs.
Healthcare technology is crucial for enhancing patient outcomes, streamlining processes, reducing medical errors, and lowering costs. From advanced diagnostics to telehealth and AI, the innovations discussed at pioneer-technology.com are shaping a more efficient and safer healthcare landscape.
Ready to dive deeper into the world of healthcare technology? Visit pioneer-technology.com to explore our comprehensive articles, in-depth analyses, and the latest updates on groundbreaking technologies transforming the medical field. Don’t miss out on the insights that can help you stay ahead in this rapidly evolving industry.
Address: 450 Serra Mall, Stanford, CA 94305, United States
Phone: +1 (650) 723-2300
Website: pioneer-technology.com
FAQ
1. What is healthcare technology?
Healthcare technology encompasses a wide range of tools, equipment, and software designed to enhance healthcare delivery, improve patient outcomes, and streamline healthcare processes. It includes everything from advanced diagnostic imaging and robotic surgery to telehealth platforms and electronic health records.
2. How does healthcare technology improve patient safety?
Healthcare technology enhances patient safety by reducing medical errors through systems like computerized physician order entry (CPOE) and bar code medication administration (BCMA). These technologies automate processes, provide real-time alerts, and ensure accurate medication management, minimizing the risk of errors.
3. What role does telehealth play in modern healthcare?
Telehealth plays a critical role in modern healthcare by improving access to care, particularly for patients in rural or underserved areas. It enables remote consultations, chronic condition monitoring, and timely interventions, reducing the need for in-person visits and hospital admissions.
4. How does AI contribute to better diagnostics in healthcare?
AI contributes to better diagnostics by analyzing medical images and patient data with greater speed and accuracy than human clinicians. AI-powered tools can detect subtle anomalies and patterns, leading to earlier and more accurate diagnoses, especially in fields like radiology and oncology.
5. What are the benefits of using electronic health records (EHRs)?
EHRs offer numerous benefits, including improved data management, reduced administrative costs, and enhanced care coordination. By providing clinicians with instant access to patient information, EHRs streamline workflows and support more informed decision-making.
6. How can big data analytics improve healthcare outcomes?
Big data analytics improves healthcare outcomes by enabling personalized medicine, improving population health management, and enhancing clinical research. By analyzing vast amounts of patient data, healthcare providers can identify patterns, personalize treatment plans, and develop more effective interventions.
7. What is the Internet of Medical Things (IoMT)?
The Internet of Medical Things (IoMT) refers to the network of connected medical devices and sensors that collect and transmit data to healthcare providers. IoMT devices enable continuous patient monitoring, real-time feedback, and remote management of chronic conditions, improving patient outcomes and reducing healthcare costs.
8. How are augmented reality (AR) and virtual reality (VR) used in healthcare?
AR and VR technologies are used in healthcare for medical training, patient education, and therapeutic interventions. AR enhances surgical precision and provides simulated training environments, while VR offers immersive experiences for pain management, rehabilitation, and mental health therapy.
9. What is the potential impact of blockchain technology on healthcare?
Blockchain technology has the potential to improve data security, interoperability, and transparency in healthcare. It can be used to securely store and share patient medical records, track pharmaceuticals, and manage clinical trial data, enhancing trust and efficiency in the healthcare ecosystem.
10. How does healthcare technology reduce healthcare costs?
Healthcare technology reduces healthcare costs by improving efficiency, preventing hospital readmissions, and enabling remote monitoring and virtual care. By automating processes, reducing errors, and providing cost-effective alternatives to in-person visits, healthcare technology helps to lower overall healthcare spending.